LAB 6 : MICROBIOLOGY
Part 1: Aseptic Technique
1.0
OBJECTIVE
1)
To produce isolated colonies of an organism on an agar plate and useful when we
need to seperate organisms in a mixed cultures
2) To identify bacteria are only valid when
performed on pure cultures.
1.1 INTRODUCTION
The hands
are the parts of the human body that are in most contact with the outside
world. People use their hands for a variety of activities everyday. It is
extremely easy to come in contact with different microbes and to transfer them
to other objects and maybe even people. Handwashing is thought to be effective
for the prevention of transmission of pathogens. There are many products in the
market claim to be able to kill the germs. However it is not conclusive that
handwashing with soap or other cleaning products is more effective at reducing
bacteria contamination than using water only.
1.3
MATERIALS/ APPARATUS
1.Bacteria
2. Loop
3. Bunsen burner
4.Alcohol
5. Agar plate
6. Ethane
1.4 METHODOLOGY
(A) Streak plate technique
1. The inoculating loop was sterilize in the bunsen burner by putted the
loop into the flame until it is red hot. Allow it to cool.
2.
An isolated colony was picked
from the agar plate culture of (a) E.
coli and (b) S. aureus and each
of them was spread over the first quadrant on separate agar plate.
3. The agar
plate was cover with the lid and flame the loop.
4.
The plate was turned and lightly
streak into the next quadrant without overlapping the previous streak.
5. Step 3
and 4 was repeated and streak into the third quadrant.
6. Each
plate was seales with parafilm.
7. The
plates was inverted and incubated at 37oC for 24
hours.
Part 1: Aseptic Technique
1.0 OBJECTIVE
1) To produce isolated colonies of an organism on an agar plate and useful when we need to seperate organisms in a mixed cultures
2) To identify bacteria are only valid when performed on pure cultures.
1.1 INTRODUCTION
Bacteria are everywhere, and some are good for
us while others are harmful. Bacteria, viruses, and other
microorganisms that cause disease are called pathogens. To protect patients
from harmful bacteria and other pathogens during medical procedures, healthcare
providers use aseptic technique.
An acid/base titration can be monitored with an
indicator or with a pH meter. In either case, the goal is to determine the
equivalence point of the titration. This is the point at which enough titrant
has been added to the analyte to just exactly neutralize the analyte.
In this experiment, knowledge of the equivalence point
will be used to obtain information about the acid dissociation constant, Ka, of
the acid being titrated. When an indicator is used in a titration, the color
change occurs at what is called the endpoint. If the indicator has been
properly selected, this point will be the same as the equivalence point. When a
pH meter is used, the pH of the solution is recorded as the titrant is added.
The pH versus the volume of titrant added can be plotted on what is called a
titration curve. In this case the equivalence point occurs at the point where
very small additions of titrant cause a very rapid rise in the pH.
The hands
are the parts of the human body that are in most contact with the outside
world. People use their hands for a variety of activities everyday. It is
extremely easy to come in contact with different microbes and to transfer them
to other objects and maybe even people. Handwashing is thought to be effective
for the prevention of transmission of pathogens. There are many products in the
market claim to be able to kill the germs. However it is not conclusive that
handwashing with soap or other cleaning products is more effective at reducing
bacteria contamination than using water only.
1.3
MATERIALS/ APPARATUS
1.Bacteria
2. Loop
3. Bunsen burner
4.Alcohol
5. Agar plate
6. Ethane
1.Bacteria
2. Loop
3. Bunsen burner
4.Alcohol
5. Agar plate
6. Ethane
1.4 METHODOLOGY
(A) Streak plate technique
1. The inoculating loop was sterilize in the bunsen burner by putted the
loop into the flame until it is red hot. Allow it to cool.
2.
An isolated colony was picked
from the agar plate culture of (a) E.
coli and (b) S. aureus and each
of them was spread over the first quadrant on separate agar plate.
3. The agar
plate was cover with the lid and flame the loop.
4.
The plate was turned and lightly
streak into the next quadrant without overlapping the previous streak.
5. Step 3
and 4 was repeated and streak into the third quadrant.
6. Each
plate was seales with parafilm.
7. The plates was inverted and incubated at 37oC for 24 hours.
7. The plates was inverted and incubated at 37oC for 24 hours.
(B) Effect of handwashing on bacteria on thumb
1. 4
nutrient agar and label them:
a) control
b) water
c) hand
sanitizer
d) soap
2.
Each agar plate was divided into
4 sections by drawing line using a marker pen on the back of the petri dish.
3. Aseptic
technique was applied, press thumb on the control
agar plate gently.
4. Hands was
washed (including thumb) with water and step 3 was repeat on the appropriate
agar.
5. Step 4 was
repeated by using hand sanitizer and soap.
6. Each
plate was sealed with parafilm.
1.5 RESULTS
Part A: Streak plate technique
1.6 DISCUSSION
The streak plate
procedure, a mixture of cells is spread over the surface of an agar medium in
the petri dish such that fewer and fewer bacterial cells are deposited at
widely separated point on the surface of the medium and following incubation
develop into colonies. Label around edge
of the bottom of an agar with at least name, the date and the type of the
organism to be plated on the medium. The last process is to place the plate
into incubater. The plate can not be left in more than 24 hours because the
colony in the plate will spread and fill the plate.
The
plate is divide into four parts namely control, hand senitizer, water and soap.
The plate has to divided because it can distinguish where the bacteria will
appear with much. The proper hand washing technique is applied in the soap
section to make sure the bacteria at our hand are clean as well. From the
result, the hand washing experiment indicate that washing with hand sanitizer
is more effective. In addition, washing
with soap appeared to be effective also but initially lagged in removing
microorganisms. One reason for this lag may be that the soap was effective in
loosening the microorganism at deeper layers of the epidermis.
1.7
CONCLUSION
Part 2 : Gram Staining
The Gram
stain is a differential stain commonly used in the microbiology laboratory that
differentiates bacteria on the basis of their cell wall structure. Most
bacteria can be divided into two groups based on the composition of their cell
wall:
2.1 OBJECTIVES:
2.2 APPARATUS AND EQUIPMENTS
- Glas side
- Loop
- Bunser burner
- Sample
- Distilled water
- Alcohol
- Iodin
- Cyrstal violet
- Safranin
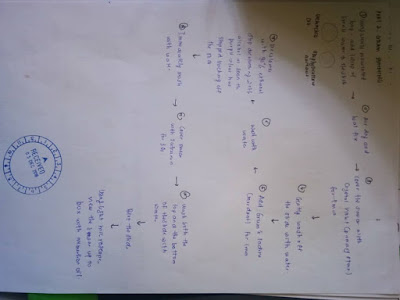
2.3 METHODOLOGY:
1.
A sterile used inoculating loop, 1
drop was added of sterile water to the slide. Prepare a smear of:
(a)
Escherichia coli and
(b) Staphylococcus aureus
2.
Dried air and fixed the heat.
3.
The smear was covered with Crystal
Violet (primary stain) for 1 min.
4.
The slide wash off with water
gently.
5.
Gram’s Iodine was added (mordant)
for 1 min.
6.
Wash with water.
7. Decolorized with 95% ethanol. This
is the "tricky" step. Stop decolorizing with alcohol as soon as the
purple color has stopped leaching off the slide (time will vary depending on
thickness of smear). Immediately wash with water. Be sure to dispose of all
ethanol waste in the appropriately labelled waste container.
8.
The smear was cover with Safranin
for 30 seconds.
9.
Both the top & the bottom was
wash of the slide with water.
10.
The slide was bloted.
11.
Light microscope used, view the
smear up to 100x with immersion oil.
2.4 RESULT
FOR E.COLI
E.Coli 10x
E.coli 40x
E.coli 100x
FOR
STAPHYLOCOCCUS AUREUS
Staphylococcus aureus 4x
Staphylococcus aureus 10x
Staphylococcus aureus 40x
Staphylococcus aureus 100x
2.5 DISCUSSION
By
using gram staining, there are two type of bacteria that exits in the slide
which is staphylococcus aureus and Escherichia coli. We used the bacterial
colony in the spread plate for staining.
2.6 CONCLUSION
2.7
REFERENCES
1)
Wise,
K. Preparing Spread Plates Protocols (2006) . Retrived from http://www.microbelibrary.org/index.php/component/resource/laboratory-test/3085-preparing-spread-plates-protocols
(B) Effect of handwashing on bacteria on thumb
1. 4
nutrient agar and label them:
a) control
b) water
c) hand
sanitizer
d) soap
2.
Each agar plate was divided into
4 sections by drawing line using a marker pen on the back of the petri dish.
3. Aseptic
technique was applied, press thumb on the control
agar plate gently.
4. Hands was
washed (including thumb) with water and step 3 was repeat on the appropriate
agar.
5. Step 4 was
repeated by using hand sanitizer and soap.
6. Each
plate was sealed with parafilm.
7. The
plates was inverted and incubate at 37oC for 24
hours
1.5 RESULTS
Part A: Streak plate technique
1.6 DISCUSSION
The streak plate
procedure, a mixture of cells is spread over the surface of an agar medium in
the petri dish such that fewer and fewer bacterial cells are deposited at
widely separated point on the surface of the medium and following incubation
develop into colonies. Label around edge
of the bottom of an agar with at least name, the date and the type of the
organism to be plated on the medium. The last process is to place the plate
into incubater. The plate can not be left in more than 24 hours because the
colony in the plate will spread and fill the plate.
The
plate is divide into four parts namely control, hand senitizer, water and soap.
The plate has to divided because it can distinguish where the bacteria will
appear with much. The proper hand washing technique is applied in the soap
section to make sure the bacteria at our hand are clean as well. From the
result, the hand washing experiment indicate that washing with hand sanitizer
is more effective. In addition, washing
with soap appeared to be effective also but initially lagged in removing
microorganisms. One reason for this lag may be that the soap was effective in
loosening the microorganism at deeper layers of the epidermis.
1.7
CONCLUSION
The conclusion is streak plate method
is one of the most common method for the isolation of pure culture of all
microorganism. For the effect hand washing, we can conclude that by using hand
sanitizer is most effective than the other method of hand washing.
Part 2 : Gram Staining
.
2.0 INTRODUCTION
The Gram
stain is a differential stain commonly used in the microbiology laboratory that
differentiates bacteria on the basis of their cell wall structure. Most
bacteria can be divided into two groups based on the composition of their cell
wall:
1) Gram-positive
cell walls have a thick peptidoglycan layer beyond the plasma membrane.
Characteristic polymers called teichoic and lipoteichoic acids stick out above
the peptidoglycan and it is because of their negative charge that the cell wall
is overall negative.
These
acids are also very important in the body’s ability to recognize foreign
bacteria. Gram-positive cell walls stain blue/purple with the Gram stain.
2) Gram-negative cell
walls are more complex. They have a thin peptidoglycan layer and an outer
membrane beyond the plasma membrane. The space between the plasma membrane and
the outer membrane is called the periplasmic space. The outer leaflet of the
outer membrane is composed largely of a molecule called lipopolysaccharide
(LPS). LPS is an endotoxin that is important in triggering the body’s immune
response and contributing to the overall negative charge of the cell. Spanning
the outer membrane are porin proteins that enable the passage of small
molecules. Lipoproteins join the outer membrane and the thin peptidoglycan
layer. Gram-negative cells will stain pink with the Gram stain.
2.1 OBJECTIVES:
1 ) To differentiate
between the two major catagories of bacteria, gram positive and gram negative.
2) To understand how the
gram stain reaction affect gram poeitive and gram negative.
2.2 APPARATUS AND EQUIPMENTS
- Glas side
- Loop
- Bunser burner
- Sample
- Distilled water
- Alcohol
- Iodin
- Cyrstal violet
- Safranin
2.3 METHODOLOGY:
1.
A sterile used inoculating loop, 1
drop was added of sterile water to the slide. Prepare a smear of:
(a)
Escherichia coli and
(b) Staphylococcus aureus
2.
Dried air and fixed the heat.
3.
The smear was covered with Crystal
Violet (primary stain) for 1 min.
4.
The slide wash off with water
gently.
5.
Gram’s Iodine was added (mordant)
for 1 min.
6.
Wash with water.
7. Decolorized with 95% ethanol. This
is the "tricky" step. Stop decolorizing with alcohol as soon as the
purple color has stopped leaching off the slide (time will vary depending on
thickness of smear). Immediately wash with water. Be sure to dispose of all
ethanol waste in the appropriately labelled waste container.
8.
The smear was cover with Safranin
for 30 seconds.
9.
Both the top & the bottom was
wash of the slide with water.
10.
The slide was bloted.
11.
Light microscope used, view the
smear up to 100x with immersion oil.
2.4 RESULT
FOR E.COLI
E.coli 4x
E.Coli 10x
E.coli 40x
E.coli 100x
FOR
STAPHYLOCOCCUS AUREUS
Staphylococcus aureus 4x
Staphylococcus aureus 10x
Staphylococcus aureus 40x
Staphylococcus aureus 100x
2.5 DISCUSSION
By
using gram staining, there are two type of bacteria that exits in the slide
which is staphylococcus aureus and Escherichia coli. We used the bacterial
colony in the spread plate for staining.
The slide
was heated because heating enables coagulation and precipitation of protein of
bacteria to occur, hence fix the bacteria on slide the bacteria killed and
adhere to the surface. In addition, cystal violet is added to stain everything
on slide or to stain all bacteria. The extra cystal violet dye that not binds
to cell is cleared by distilled water. Addition of iodine in next step anables
the cystal violet dye further fix and adhere to organisms. Iodine acts as
mordant as it increase affinity of cystal violet stain to organisms. The addition
of ethanol as decolourizer enables the lipid to be extracted or dissolved from
the cell wall from gram negative bacteria like the Escheriichia Coli. Ethanol was
not added for more than 30seconds because over decolourization can cause the
stain og gram positive bacteria to decolourize and appears as gram negative.
Under
microscope, staphyloccus aureus is rod-shaped and apprear in purple colour. While
Escherichia coli is rod-shaped and appear in red colour.
2.6 CONCLUSION
Gram
staining is important in differentiating gram positive and gram negative
bacteria in which the gram positive bacteria stained purple colour while gram
negative organisms stained pink. Escherichia coli is gram negative while
staphylococcus aureus are gram positive bacteria.
2.7
REFERENCES
1)
Wise,
K. Preparing Spread Plates Protocols (2006) . Retrived from http://www.microbelibrary.org/index.php/component/resource/laboratory-test/3085-preparing-spread-plates-protocols





















Comments
Post a Comment